After months of quiet on the health front in the wake of the federal election, health policy debate lit up like a Christmas tree over the festive season in response to the announcement by Health Minister Peter Dutton of the review of Medicare Locals and his surprise flagging of the possibility of co-payments for bulk-billed GP visits.
This is the first of two posts on those developments.
***
News that a co-payment for bulk-billed GP visits was on the agenda for the Federal Government’s “razor gang” – its Commission of Audit – came in a Sunday Telegraph report during the Christmas-New Year week, a real surprise from the bottom of Santa’s sack.
It noted the detailed proposal for the co-payment fee had been made in a submission to the Commission by the Australian Centre for Health Research (ACHR), in this October 2013 research paper prepared by Prime Minister Tony Abbott’s former health adviser Terry Barnes.
In this piece in The Australian, Barnes says the paper has “caused such a sudden furore that I feel I’ve grown a devil’s tail and horns”. The response can hardly have come, though, as a surprise, given the intention and implications of the proposal and, not least, Health Minister Peter Dutton’s statement, refusing to comment ahead of the Commission’s finding (a first report is due end of January, with the final scheduled for March, ahead of the May budget).
The proposal is that a $6 co-payment could significantly reduce the number of GP visits and therefore save the Federal Government $750 million over four years. Barnes provides the following policy rationale:
- “Reducing avoidable demand for GP services, particularly in outer suburban and regional areas where GPs are in relatively short supply. By helping to manage demand, GPs will be able to concentrate more of their scarce time on patients who most need treatment or care management.
- Reducing incentives for GPs to overservice where there are high concentrations of general practitioners – the principal justification of the 1991 Budget measure.
- For Unreferred Attendances (that is GP services), in which 80 per cent of services are bulk-billed, sending a price signal to consumers and reminding them that GP services are not a free good.
- Provided that co-payments are not large enough to deter people from going to the GP if that is what their health indicates, reducing moral hazard risks by making people think twice about going to the doctor about minor ailments treatable with rest and/or over-the-counter medications.
- Offering a simple yet powerful reminder that, as far as possible, we have a responsibility to look after our own health, not simply pass on all the costs of, and the responsibility for, caring for ourselves to fellow taxpayers.”
Asked whether the fee would force low income patients to present at hospitals instead, Barnes suggested it could also then be imposed by emergency departments:
Details on the level of the proposed fee itself ($5 or $6) and possible exemptions (for the first 12 GP visits or kicking in after the 12th visit) were a little confused in some of the reporting, but Barnes’ report proposes that: “Concessional patients and families with children under 16 would reach a safety net threshold after 12 visits to a GP in a year – that is, averaging one visit per month, or a maximum co-payment of $72. After that, the Commonwealth would pick up the full cost of GP visits for the rest of the year, including the co-payment equivalent.”
The proposal, of course, has some support (not just from the Institute of Public Affairs, which described opposition as self-serving). Health economist Ian McCauley says (in more detail below) that the proposal is poor public policy as it stands, but that a co-payment shouldn’t be ruled out by “knee-jerk outrage” as it was in 1991 when it was first proposed but then dropped by the Labor government.
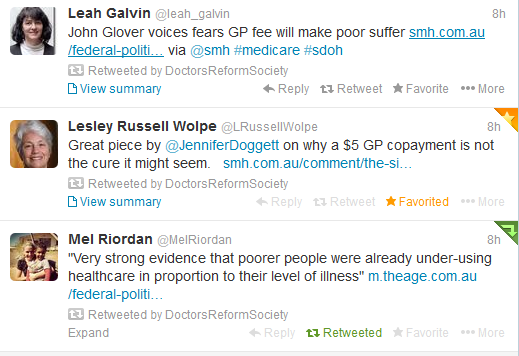
But the overwhelming response from public health experts and peak bodies including the Australian Medical Association was alarm that it would disproportionately affect poor patients, who already are not using primary care as much as they need and end up more frequently at the crisis end of care, and the repercussions generally for primary prevention policy. There’s also concern about the mechanisms and administrative hassles for collecting such a fee, and its potential to rise over time.
University of Adelaide expert on health inequality Professor John Glover warned that that those living in the poorest neighbourhoods are more than three times more likely to delay medical consultations because of costs than those living in the wealthiest suburbs.
Researcher Gemma Carey pointed to this review of co-payments across the OECD which confirmed they lead to lower uptake of services by the poor and, in Canada, actually increased uptake by the wealthy – “so widening social and health inequalities in a very active way”. This study found that raising cost sharing for ambulatory care among elderly patients may have adverse health consequences and increase total spending on health care.
As well as outlining the potential impact on vulnerable people, Dr Tim Woodruff from the Doctors Reform Society raised concern about what starts as a “modest’ co-payment: “The PBS in 1971 was $1. By 1979 it was $2.75. It is now $36.10.”
Read more responses below, including detailed assessments from Croakey contributors.
Prof Kerryn Phelps on Medicare’s identity crisis:https://ultimatewellness.net.au/blog/
Health plan the cruellest cut by Lesley Russell
The side effects of GP co-payments by Jennifer Doggett
Dr Tim Woodruff, Doctors Reform Society
The impact of a co-payment on patients would be, as has been stated elsewhere in the last few days by many, decreased service use leading to increased costs elsewhere, either in Emergency Departments or hospitals and specialist services when patients end up there because they have had inadequate primary health care. This would include immediate serious problems such as severe asthma or acute complicated diabetes, long term preventable problems such as diabetes and heart disease, the disaster of missing early diagnosis of easily treatable cancer, and the potential to intervene early in so many mental health conditions which are already in many cases badly managed by an under-resourced health system.
In the long term co-payments are simply a way of pursuing the long term neoliberal agenda of a user pays health system for all but the most disadvantaged who will receive the benefits of a second rate safety net. This will not impact on the affluent; the main impact will be felt by the poor and their children.
In terms of price signals and deterring use of services, whether necessary or unnecessary, Australia ranks third in the OECD for patients paying more than US$1000 per year for out of pocket costs.
The myth that ‘we need a system of individual contributions’ for health care continues to be promulgated even by those who recognise that a $5 GP co-payment is silly and overuse of GP services is probably overated. This idea is about user pays. We don’t have user pays to get a police or fire service response, or to use most roads or to get help from our local member about a specific concern, although corrupt politicians like the idea. In fact we already have individual contributions for all these services. They are called taxes. Rather than user pays, everyone pays according to their capacity to pay rather than how much they need. As a community we share the burden. That was always the idea behind Medicare and it has been constantly attacked since its introduction.
The second myth being promulgated is that individual contributions are necessary for patients to value the service. My bulk billed patients still bring me gifts. They value the service I provide. Some may not, but some who pay also don’t appreciate the service.
See more: A new tax on illness
Stephen Leeder, Professor of Public Health and Community Medicine at the Menzies Centre for Health Policy and School of Public Health, and Editor-in-Chief, Medical Journal of Australia
There is adequate empirical evidence to show that a co-payment at the time of use of a service creates a barrier for those least able to afford it and that poorer health outcomes follow for this group.
So knowing that, we can only assume that the current Government considers the financial situation with the national budget to be so desperate that the poor must miss out on services to help fix the deficit – not the rich, for whom a co-pay is NOT an impost. Given these facts we can conclude that the current Government does not mind increasing inequity of access to health care.
We have residents in the suburbs of Mt Druitt who cannot attend the polyclinic because they cannot afford the bus fare. So the co-pay for bulk billing will be just great for them, won’t it.
Ian McAuley, health economist
The Commission of Audit’s proposal to charge a $5 or $6 fee for “bulk-billed” GP services has little to commend it. But that doesn’t justify knee-jerk outrage from medical and consumer groups, or from the Labor Opposition, for there is no reason why Medicare should not incorporate fixed and limited co-payments.
As it stands the proposal is poor public policy, proposing a $6 charge in order to bring price discipline into service use but contradicting itself by suggesting those co-payments could be funded through private health insurance.
There is no explanation of principles, no system-wide view, and no consideration of the costs of handling 140 million small transactions each year.
It’s simply a proposal to save $750 million in Commonwealth outlays over four years. Why four years? Because that’s the “forward estimates” period. Why Medicare services and not all health expenditure? Because that’s the budgetary line item. Why only fiscal outlays and not total health care costs? Because fiscal considerations have taken over from economic considerations, and if the cost falls on state governments through a move to outpatient services, that’s none of the Commonwealth’s responsibility. We have a fiscal system, not a health care system, and a political imperative around the budget bottom line.
If we had a completely free health care system, the indignation of lobby groups and the Opposition would be understandable, because it would indeed be a wedge into our system. But we already pay 19 percent of our health care outlays from our own pockets (about the OECD average of 20 percent). We may have the luck to find a “bulk billing” GP, but if we have to fill a pharmaceutical prescription scrip we have to pay up to $36.10, or $5.90 if we hold a concession card, and if the suggested medication is not on the Pharmaceutical Benefits Scheme, it’s whatever the pharmacist charges. If we cannot find a bulk-billing GP (only 81 percent of GP services are bulk-billed, and they would be disproportionately for card holders), then we are paying on average $29 from our own pockets.
We don’t know the rationale behind the proposal – this Government is not given to policy openness – but it’s probably driven by the tremendous growth in use of medical services over the years. In 1984-85 we used about seven Medicare services per head, in 2002-03 we used 11, and in 2012-13 we used 15. Ageing explains some of this, but there has been growth in utilisation across all age groups. While half the population uses seven or fewer services a year, 10 percent of the population uses 31 or more services – more than one a fortnight – accounting for 44 percent of services. (These figures relate to 2007-08, so they would understate the skew to heavy users. The Department no longer publishes this data.)
Penny Wong portrayed the proposal as a disaster of Thatcheresque proportions, claiming that a $6 fee would be a barrier to access, ignoring the barriers imposed by long waits at bulk-bill clinics (many people would be spending more than $6 in parking fees), and the closed books at GP surgeries whose capacity has been absorbed by heavy users.
Oppositions criticise – that’s their job. But they shouldn’t close off avenues for possible reform. An opposition with a little nous could complain about the process issues mentioned above. “Yes, we have a problem, and we need some rationalisation of co-payments, but this is an inept and counterproductive way to go about it…”.
The political reaction is similar to what happened in 1991, when the Hawke Government proposed fixed co-payments. The squeals from groups supposedly on the “left” forced the Government to a hasty retreat. “Medicare” became implanted in the political and public mind as a “free” primary care service. (Earlier, in 1987, the Coalition had abandoned their plans for people to spend $250 before receiving Medicare support, because of similar protests.) In 1991 the most common protest was that Medicare would become a “safety net” rather than a universal free service.
The gaping flaw in that protest is that we have never had a universal free health care service.
In those campaigns of last century the “left” exhausted its political energy defending free Medicare services. But what has developed, a resurgence of private health insurance, is far worse by any reasonable criteria of equity or allocative efficiency. As for the protests about a safety net, a safety net would be far better than our inconsistent arrangements which leave people, particularly those with chronic illnesses, bearing open-ended liability for uncapped expenses.
There are three ways to fund health care – direct consumer payments, a single national insurer, and competing private insurers. Two of these mechanisms – one a market mechanism, one a countervailing power mechanism – can keep health care costs in check and assure there is universal access to affordable services. The third mechanism, private health insurance, fails to achieve these outcomes and leads to price inflation and inequity. Its elimination should be the focus of consumer and Opposition energies.
Why should any consumer group or a party aspiring to government rule out one of the two mechanisms that actually have a chance of working?
Dr Gemma Carey, Centre of Excellence in Intervention and Prevention Science (CEIPS)
This review of co-payments compared countries across the OECD and found, as one would expect, that they tend to lead to lower uptake of services by the poor, making them a false economy. Interestingly, the review found that, in Canada, the co-payment increased uptake by the wealthy – so widening social and health inequalities in a very active way, which is, of course, bad for everyone. If adopted by the Abbott Government, it would signal a further shift away from its liberal wing, cementing it as a neo-conservative party that gives preferential treatment to the wealthy at the expense of the poor.
Tim Senior, Sydney GP
There’s been quite a bit of commentary on the idea of a co-payment for GP Services, most of it unfavourable, though some supportive. The angles have been correct – that it affects most those who can least afford it – but even this overlooks the extent of the problem and implies an even distribution of disease burden across the community and an even distribution of wealth geographically. In fact, because people with low incomes have worse health problems, they are affected twice over by such a proposal.
On a personal note, almost all of my patients have been put off doing something favourable to their health – usually a prescription – because of a small cost. This Lancet paper shows multi-morbidity coming in 10 years earlier for the most deprived.
My second point, which I haven’t seen mentioned at all in current commentary, is that there is huge potential for the measure to de-fund primary care in deprived areas, because those who can least afford the co-payment tend to live in similar suburbs. GPs in richer areas who don’t currently bulk bill will continue not to bulk bill. GPs in poorer areas who do bulk bill will either charge the co-payment and have many patients who can’t see them, or have to waive the co-payment so people get access to care. But they will be doing this for a large number of their patients, as they are all in similar situations. The practice will have to absorb these hits to their income and so have fewer resources to manage the more complex physical, mental and social problems they are faced with.
Alison Verhoeven, Chief Executive, Australian Healthcare and Hospitals Association (AHHA)
Overall my concern is that the proposals being mooted are very blunt instruments aimed at achieving a fiscal goal (which may not be realised, due to the flow-on effects, see further below) and which will particularly hurt those most in need of support (people with chronic illness, on low incomes). This is particularly concerning because it also interacts with other mooted changes such as the scrapping of the net medical expenses tax offset, and with the recently announced 6.2 per cent private health insurance premium increase.
These measures seem to be quick fixes aimed at plugging fiscal holes rather than based on sound evidence (for example, is there sufficient evidence to demonstrate over-use of services which appear to be without cost, noting that taxpayers do contribute to cost in any case?; what evidence is there that the $6 price-point is the most appropriate to minimise overuse without causing undue social harm?). The government should also ensure that this major health policy shift is taken with some consideration of the broad interaction between public and private health – and I suggest that it would be timely to review this with more rigour, rather than to implement changes at the fringes as the result of ideologically-driven lobbying.
Social impact seems to be totally overlooked in the Australian Centre for Health Research proposal.
It raises particular concerns for those with chronic illness and people on low incomes, who may either not see a doctor when they need to, potentially becoming more ill and requiring more services including hospital care; or who may divert to emergency departments for care which would be better and more cost-effectively delivered by GPs.
The second proposal to charge a co-payment for Emergency Department services is fundamentally worrying – citizens as taxpayers have the right to expect some basic services to be covered out of their investment via taxes. That this should include emergency healthcare would be a priority for most Australians, possibly more so than many other areas of government expenditure.
A sustainable high quality health system is a goal we must aspire to – but the path to sustainability mustn’t be at the cost of providing basic services to people in need. There are a range of measures such as a disinvestment strategy, value-based fee models versus fee for service, alternative workforce models, which deserve more consideration from a government seriously committed to a world class health system.
Alf Liebhold, GP
The health care costs which have exploded most dramatically in recent years are those involving laboratory investigations, radiology and specialist referrals.
One of the main reasons for this explosion is the tendency for GP consultations to be too short and superficial. The reason for this is financial: longer consultations are uneconomical for a GP as they are not rewarded in proportion to standard or short consultations.
If the longer consultation were appropriately rewarded relative to its time expenditure, GPs would be encouraged to take a more complete history and get to know the client’s personal history. By this simple change much laboratory and radiology work could be better targeted and often be shelved at least for some time while the condition was being monitored.
I speak from 55 years’ experience and I dare say that my investigation and referral rates have been well below average. The reason is that I take time to acquaint myself with the presenting situation and accept an inevitable income loss as a result. But this approach is difficult to recommend to younger colleagues with mortgages and family expenses.
Summing up: If longer consultations were rewarded appropriately, better and less expensive medical care could be achieved.
Elizabeth Harris, Senior Research Fellow at the University of NSW
What is the policy trying to achieve? It appears that this policy initiative is attempting to contain rising health costs through reducing costs and use of GP services.
What is the evidence that use of GPs is a major driver of increased health costs? There are about 100 million visits to GPs per year. A $5 levy on each visit would raise $500 million assuming non-bulk billing GPs also raise co-payments. Total Medicare expenditure is $18 billion, $12.4 billon of which is bulk billed. This would have limited impact overall costs. There was about a 3 per cent increase in Medicare services in 20120-13 and 4.5 per cent increase in costs compared to the previous year.
Co-payments reduce demand for care. Introduction of a co-payment on bulk billing may reduce demand for GP services and this may in turn reduce test ordering (covered by Medicare) and prescribing (covered by the Pharmaceutical Benefits Scheme which cost around $9 billion in 2012/13) by GPs. Thus the net savings may be greater than the amount the $5 levy would itself raise.
The introduction of a co-payment may also increase pressure for private health insurance to be able to cover this and other gaps in medical payments (they are currently not able to cover gaps in non inpatient costs). If this occurred it may tend to erode the role of Medicare as funder and its ability to contain medical costs.
Fixed co-payment disproportionally affects low income groups. Older people and those with chronic conditions make more frequent visits to GPs and would thus bear greater costs.
Is there any evidence that increased co-payment it is likely to work? There is evidence that countries with strong primary health care services have lower costs and better health outcomes. A key component of an accessible health service is affordability. Co-payments can reduce demand but have most impact low income groups who also have poorer health.
Who are likely to be the losers?
- People with limited disposable income who are also the people more likely to have complex health problems and co-morbidity are most likely to have reduced use of services or trade-off health care for other expenditure ( food, clothing etc).
- The Australian population through potential reduction in access when needed
- GP practices that are likely to have additional administrative work and high transaction costs in collecting cash.
What might be unintended consequences?
- Increased use of hospital emergency departments ( ironically, the Commonwealth is currently investing heavily in strategies to reduce emergency department use).
- Increased admissions to hospitals due to poorer and delayed management of preventable admission.
On the proposal to charge a similar fee to emergency department visits, the problem is the cost of building or scaling up a billing infrastructure. And is this where the problem is based and is billing the best solution? For example, residents of aged care facilities are high users of after hours emergency departments. How will they pay? Recent initiatives to provide more support to nursing homes via Medicare Locals have been successful in some places in reducing demand.
Recommendations:
- Properly assess the major causes of rising health care costs and target policy initiatives at these causes – including cost shifts between state and commonwealth.
- Protect a strong universal primary health care service.
* To comment on this story, visit the original post at our health blog Croakey











Crikey encourages robust conversations on our website. However, we’re a small team, so sometimes we have to reluctantly turn comments off due to legal risk. Thanks for your understanding and in the meantime, have a read of our moderation guidelines.