Australia has nearly 9 million COVID-19 vaccines onshore. The vaccine supply chain line is long, convoluted and involves expensive private contractors to oversee, advise and staff the rollout.
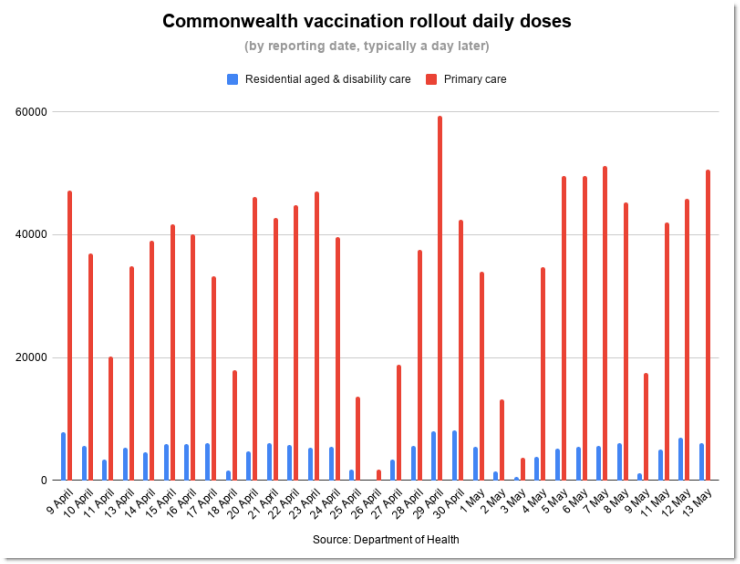
Just 2.89 million of those doses have made it into arms — and just 279,000 of those are in residential aged or disability care. Just 11% of Australians have received their first dose. Australia ranks 34 out of 37 OECD countries for single doses per 100 people.
The slow vaccination rate is expected to push back our border opening well into next year, keeping families apart and causing a huge hit to the economy.
There’s no one single problem but a series of issues that include:
- An over-reliance on AstraZeneca versus other vaccine candidates
- Relying on a single manufacturer to produce most of our doses
- Crucial but slow testing of vaccines batches
- Issues with delivery leading to wasted doses
- Poor risk management and administrative mistakes leading to low public confidence in the vaccine
We backed the wrong vaccine horse
Australia backed the wrong vaccine horse. Our major vaccine Novavax, of which we ordered 61 million doses, is still in phase three clinical trials. We initially only secured 10 million doses of Pfizer, with another 30 million doses on backorder, and 53.8 million doses of AstraZeneca. We were also betting on the University of Queensland vaccine, which was abandoned after causing false positive HIV results.
Our reliance on the AstraZeneca vaccine has proven problematic. It has a lower efficacy rate of about 70% compared with Pfizer’s 95%, and links to cases of blood clotting have led to doctors warning about vaccine hesitancy.
Government forecasts released in March (which have since been abandoned) showed Australia expected to have 20-25 million doses by now. Instead, we have 8.8 million doses — 2.3 million of Pfizer and 6.5 million of AstraZeneca.
While manufacturers around the world are facing delays caused by disruptions in supply chain lines, shortages of primary materials, and new COVID waves disrupting staffing, most of Australia’s Moderna, Pfizer and Novavax doses were always earmarked to arrive in late 2021. Just one shipment of the AstraZeneca vaccine for Australia was blocked by the EU amid shortages, contrary to Prime Minister Scott Morrison’s claims.
We’re relying on one manufacturer
Onshore manufacturer CSL had to pivot from manufacturing the planned UQ vaccine to AstraZeneca in December. It’s one of the few onshore drug manufacturers in Australia, with other facilities lying dormant after years of relying on overseas production.
According to February forecasts, CSL was expected to have produced 7 million doses of AstraZeneca by mid-May although data provided by the Health Department to Crikey shows it has produced only 5.5 million doses (with around 1 million doses having been imported). CSL only started manufacturing 1 million doses a week two weeks ago, a month behind schedule.
CSL tells Crikey biological manufacturing requires fine-tuning, with variables affecting the number of doses produced in each batch, but that it is now delivering targeted volumes.
As revealed in Tuesday’s budget, the government plans to develop onshore mRNA vaccine manufacturing capability — a new form of vaccine technology used for Pfizer and Moderna. Opponents have slammed the government for waiting until the eleventh hour, while exactly how much money has been committed is unknown.
Testing takes a month
Doses produced by CSL, along with those arriving from abroad, are tested by Therapeutic Goods Administration (TGA). Last week the TGA released 351,000 doses of Pfizer and 736,900 of AstraZeneca. The Health Department didn’t respond to Crikey’s questions about how many doses the TGA can test in a week, and whether this is causing a bottleneck in the supply chain.
Delivery is disjointed and ad hoc
Once approved, the vaccines are sent to 5227 vaccination sites, consisting of vaccine hubs, GP clinics and Aboriginal community-controlled health services by the Commonwealth’s Vaccine Operations Centre. This is how it works for the influenza vaccine, but with an added challenge: Pfizer has to be stored between -90 and -60 degrees, although can be kept at domestic freezer temperatures for up to two weeks. Hospitals generally have this capacity, but GP clinics don’t.
Consulting firm PwC is the federal government’s delivery partner for the vaccine rollout and DHL Supply Chain and Linfox are operating the national distribution network. Exactly what they’re doing — and how much they’re being paid — remains secret.
Delivery hasn’t gone smoothly. Doses have been thrown away because of late or cancelled shipments breaching the cold chain, with doctors complaining of doses not arriving.
Confidence is waning
The Commonwealth is in charge of vaccinating aged and disability residential care residents with states vaccinating the general population. The Commonwealth contracted four private companies to organise the workforce — Aspen Medical, International SOS, Healthcare Australia and Sonic Healthcare — and there have been problems in delivery, from doctors not being trained to residents vaccinated without consent while those ineligible have been able to book themselves in for a vaccine.
This, combined with concerns around the adverse effects of the AstraZeneca vaccine and its efficacy, has seen a growing number of Australians lose confidence in the rollout.
There’s no single failure in the distribution line. Rather, a combination of problems means Australians can’t expect to be vaccinated as quickly as we had hoped. The Health Department denies there has been a delay in distributing the vaccines.








I think it was only the men in Cabinet who were vaccinated. The women have to wait. They also sent a woman to face the guns on Q and A last night. None of the big swinging dicks had the guts.
That’s crazy talk.
Don’t look at me.
“Australia” didn’t “back the wrong vaccine horse” – Oz punters designated Scotty from Marketing to handle the bets for our Punter’s Club – it was him and his weasels that blew it on that AstraZeneca-Novavax quinella.
Picking winners? They couldn’t pick their noses without a manual.
But that’s digital.
Or stickin’ up for your mates.
And again I am reminded of my dear old Scots Gran. “Could nae run a bath!”
As I have said before: if we had a well-staffed, skilled and experienced Health Department running the show instead of overpaid management consultants, the rollout etc would have proceeded much more smoothly. But they still don’t get it. Some LNP politicians are complaining about the projected increase in public servants in the Budget.
And is Greg Hunt and his Health Dept. flunkies going to take responsibility when the targetted older people start dropping like flies with clotting issues after being exhorted to have the AstraZeneca vaccine? Mind you, the LNP cabinet all lined up for the Pfizer jab at the head of the queue; no AZ for them…
Was it all of the Cabinet, or only the PM? BTW, who is the rest of the Cabinet?
“flunkies going to take responsibility when the targetted older people start dropping like flies with clotting issues after being exhorted to have the AstraZeneca vaccine?”
Says it all. But it’s just not older people.
“Mind you, the LNP cabinet all lined up for the Pfizer jab at the head of the queue; no AZ for them…”
They’re welcome to it – see my post below & take the time to visit site to read some sceptical medical info.
You do realise that 100’s of millions of AZ vaccine have been administered world wide don’t you?
“Dropping like flies” is a callous, untrue and emotive piece of nonsense.