Medicare is ill-equipped for 21st century doctor and patient needs, a new Grattan Institute report has found. It recommends a drastic overhaul of Australia’s universal healthcare system to fix the frontline of general medicine and bring it up to speed with the country’s growing caseload of chronic disease.
The report paints a grim picture of general medicine in which GPs are harder to access, patient numbers are up, and presentations are increasingly acute and complex. Patients need more time with GPs who are being encouraged to move in the opposite direction and trim down consultations.
The institute points to a lack of human resources and funding.
“Australia has spent 25 years on a merry-go-round of tests and trials that have not changed the system, and our rates are holding steady,” the report said.
So what’s different about this approach?
Much of the conversation has centred around the need for attracting and retaining more doctors. The report acknowledges that GP numbers are down (or absent) in rural regions but finds this to be an issue with distribution rather than a lean workforce. Australia’s GP per person ratio is higher than most wealthy countries.
The bigger problem, noted in the report, is that general medicine is modelled on individual doctors serving individual patient needs. One of the institute’s key recommendations is to turn general medicine into a “team sport”.
Australia’s current regulatory and funding set-up encourages lone operators, but the report finds that instituting a bit of workplace hierarchy would go a long way.
In short: better primary patient care and follow-through.
GPs make up about 74% of the clinical staff in Australian general practices and yet for every 10 GPs there are fewer than three nurses or other clinicians to support them. Compare that with England, which is at a ratio of 1:1 of GPs to supporting clinicians.
In Australia, GPs do all the work, with supporting staff delivering close to 0% of primary care. The US (a health system Australia prides itself on beating in every way) allocates about 11% of the workload to nurse practitioners and physician assistants.

General practice is deemed the “best place to tackle chronic disease”, but the report finds funding continues to favour the hospital system.
All patients and doctors suffer as a result, but poorer Australians are disadvantaged the most — they are twice more likely than a wealthy Australian to have a chronic health problem.
The authors note the system is in crisis and reform is “overdue” but an opportunity has arrived in the $250 million set aside by the federal government to respond.








Yes, but society has moved on since Medicare was envisaged and implemented.
If all older Australians returned to the body fat percentage they had back when Medibank was established the pressure on Medicare would be manageable.
We should be aiming for a population that has minimal chronic disease rather that planning economic treatment structures for people who have adopted a chronic disease-inducing lifestyle – that is, well before pain and dysfunction lead them into a GP’s office. And it does not follow that GPs have to be at the centre of such a reform.
Should be central to school curricula and public education for adults via media, but therein lies the problem, up against the same ;freedom & liberty’ models used by fossil fuels, tobacco etc..
Sectors with funding, junk science, PR, lobbying and consolidated media access such special interest corporate groups have e.g. beverages, fast food, food labelling etc., then general understanding, or not, of food/health science and promoting activity.
Not sure all of them can, since life expectancy then was just over 70 and it’s now over 83 and increasing. Of course, we could ask them all to kindly go back to shuffling off this mortal coil at 71 and take some chronic diseases of ageing burden off Medicare that way.
That is effectively what the federal government is hoping will happen whilst they sit on the latest vaccine until winter, when blind freddy could tell you that Covid19 is not really associated with winter, like influenza is.
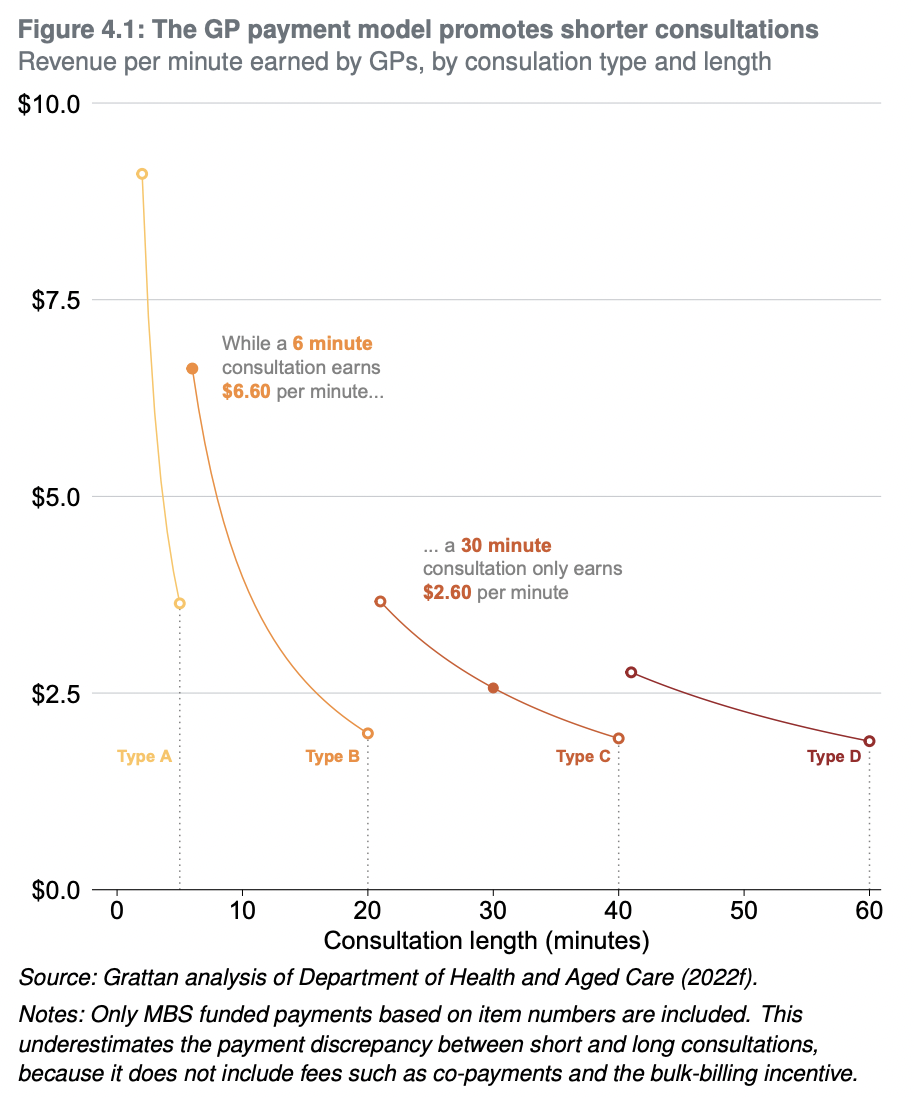
Well done to the Grattan Institute for telling everyone what has already been known for decades. The current GP fee structure actively encourages shorter consultations. It is far more remunerative for a GP to listen to a patient for 4.5 minutes, spend 30 seconds writing out a script, spend 30 seconds telling the patient how to take what has just been prescribed, and then yell NEXT!! than it is to spend 20, 30, 45 minutes with a patient.
It is also far better to have a GP leading a team of clinicians looking after those with chronic disease than it is to leave all such management in the hands of GP shoehorned into 6 minute chunks (the simple Fee For Service model is probably still better for acute medicine). It is also plainly apparent that the relative value of a GP consultation has been eroded massively over the past two decades.
So apart from telling us what we already know, what does the report propose?
Using the UK as any form of comparison is a huge mistake. Their NHS is awful. Totally and terminally disastrous. Dreadful. Completely incompetent. To actually import any part of their system would be extremely foolish. Whatever problems Medicare has will not be fixed by copying the NHS in any way, shape or form. For starters, their GPs and nurses are not allowed to practice good, competent medicine. Choice of treatment, and even the ability to make a diagnosis, is decided by iron rules having nothing to do with health and everything to do with cost. This has led to demoralised doctors and nurses who no longer are capable of doing their job and most of them simply don’t care any more. I observed all this for six months while looking after my terminally ill sister. It was horrifying. No exaggeration. I still find it hard to believe many of the things my eyes saw. Put your trust in the NHS and death awaits. Seriously. If you are ever sick in the UK, get out immediately.
It’s your only chance.
I’ve only had a few ales ….
The NHS is patchy. I lived 2011-2020 in Cambridge and there it was consistently excellent, both for me and my aged parents in law. But Cambridge is middle class with a top university hospital.
But the NHS was designed for a population profile that the UK had in the late 1940s, so it’s bound to be “not fit for purpose” now – as the client base has evolved in every relevant parameter.
And successive governments have slashed and burnt for 25+ years …..
We might also think about why we are so sick? I note that in disaster scenarios we now have to have emergency drug dispensaries as well as food, water and accommodation provisions. How did we get so sick? Is there a symbiotic relationship between the fast food companies that makes us sick and big pharma treating our symptons to keep us alive and spending but never cured? Big business wins but vast numbers of us feel like crap all the time.
The food companies don’t make you sick unless you make the decision to buy their products and consume them – often in defiance of both common sense and expert dietary advice.
Unfortunately many people do not have ‘common sense and expert dietary advice’ vs. walls of media agitprop or advertising.
The eternal victim – “I was forced to eat & eat & eat this gunk!”
if they were simply making food and selling it you’d have a point. Now how much do they spend on lobbying, opposing regulations and deliberately misleading advertising?
How much has to do with pollution – air quality and the pervasiveness of micro plastics in absolutely everything, habitat destruction and just a increasing population density? Thanks to modern medical practices, we stay alive longer with ailments that would have killed us a few decades back, but our habitat is not conducive to healthy living. I’m the same weight I was when I was 23, but 50 yrs on, not as fit nor as capable physically, as I once was. Having just come from a medical centre however, I was just amazed at how many grossly unfit looking older people there were there. My wife and I, despite our problems, felt positively nubile.
A friend was slotted in for a major, but not urgent, operation at Westmead Women’s hospital in less than a month from first consultation which was surprising for a public patient.
The reason, she was told, was because she had an excellent prognosis – no history of other ailments, was not ‘on medication‘ (as seems to be the norm for 70yr olds?!), did not smoke or drink, was not overweight, fit and active so the investment was worthwhile.
Noticing the other patients (and companions) the point was obvious.
We had no idea of the general state of so many people as we never go to such places.
I have never consulted a doctor in my life which will soon be a problem because my next driver’s license renewal, when I am 75, will require a Fitness to Drive certificate. Annually!
We’d do better with a “wellness industry” than a “sickness industry” – the focus itself creates some of the problems. A while back I did an analysis just for fun, of ideas to reduce the cost of medical care. One of those was to introduce the concept of NNT for doctors to routinely use when treating the possible side effects of medications. NNT would help them assess whether to treat side effects or look for another way to treate the original illness. NNT is the Number Needed to Treat – the number of people needed to be treated by a drug before one person benefits. Even for some very commonly prescribed medications, it’s quite shocking. If it became fundamental to practical decision making about whether to treat side effects or look for another way, it would INcrease health outcomes AND it would save a fortune.